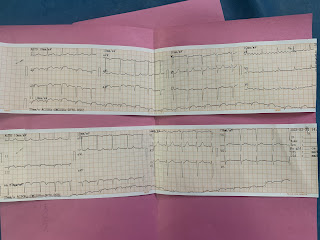
A 42 year old with HEART FAILURE WITH REDUCED EJECTION FRACTION
NAME : M. NAGA VARSHA
BATCH : 2017
ADMISSION NO. 176015
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
FOLLOWING IS THE VIEW OF MY CASE
CHIEF COMPLAINTS:
C/O left shoulder pain since morning 11am radicating to chest
C/O Shortness of breath from morning 11AM
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 11 days back he suddenly developed
-chest pain radiating to left shoulder and was associated with sweating and palpitations.
- He went to KIMS, NKP and was diagnosed with inferior wall MI + posterior wall MI. He was referred to KHL and was managed conservatively.
-Later he was asymptomatic till today morning 11AM, where he suddenly developed left shoulder pain radiating to chest(dragging type) and not associated with sweating, palpitations, nausea, vomiting, giddiness,
(ii)shortness of breath
-GRADE III - GRADE IV,
-orthopnea +
-no PND
- K/C/O CAD since 12days
PAST HISTORY
- Diet: mixed
- Appetite: increased
- Bowel habits: normal
- Bladder habits: normal
- Sleep: normal
- Addictions:
- Pallor - absent
- Icterus - absent
- Clubbing -absent
- Lymphadenopathy - absent
- Cyanosis - absent
- Pedal edema -absent
- Temperature - 98.6 F
- Pulse : 96 bpm
- Respiratory rate : 28 per minute
- Bp 100/80 mmHg
- Spo2 98%
- GRBS 122 mg%












Comments
Post a Comment