50 year old with SOB
general medicine case discussion
Makkena Naga Varsha
MBBS 9th semester
Roll no:76
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
Following is the view of my case..
- shortness of breath since 20 days
- difficulty in swallowing since 3 days
- no able to open her mouth since a day
- 10 years ago
- 8 years ago
- 6 years ago
- 5 month ago
- 4 months ago
- January
- February
- 7th march
2. cough with expectoration - mucoid, intermittent, non foul smelling
3. difficulty in opening mouth and oral ulcer is present
4. dysphagia not able to to take solids and liquids
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
Patient is moderately built and nourished.
VITALS
Temperature: Afebrile
Pulse rate:
Respiratory rate:
Blood pressure:
- diet : mixed
- apatite : normal
- bowel and bladder : regular
- sleep : adequate
- addictions : no addictions
- Alopecia - Present
- Eyes - Proptosis seen, no conjunctival suffusion
- EOM - Intact
- red tongue seen
- No thyroid swelling
- Skin - Multiple hyper pigmented macules seen all over face, upper limbs, neck, thigh, abdomen and upper back.
- Dry skin present ; Thickening of skin over forearms, dorsum of hand and fingers and on and around mouth.
- Hair is absent over the macules.
- Slight peeling is still present over the arms and legs.
- Respiratory examination:
INSPECTION: Movements of chest appears to be decreased on the left side in comparison to right side.
PALPATION: Vocal fremitus decreased in left mammary , ISA area in comparison to other areas.
PERCUSSION: Dull note in left mammary area and ISA area.
AUSCULTATION: Decreased air entry on left ISA,IMA area. Right side - normal air entry. Bilateral vesicular breathing noted. Tubular breathing heard on right inter-scapular area.
coarse crepitation - end inspiratory - no variation with cough - heard on left ISA >>right ISA.
- CVS examination:
S1,S2 heard
No murmurs. No palpable heart sounds. - Per abdomen
Inspection:Shape – normal
Umbilicus – Central, inverted
Flanks – free
Skin- no sinuses, striae are seen
Dilated veins – absent
Movements of the abdominal wall with respiration is present
No visible gastric peristalsis and no visible pulsations.
Palpation:
No local rise of temperature and no tenderness
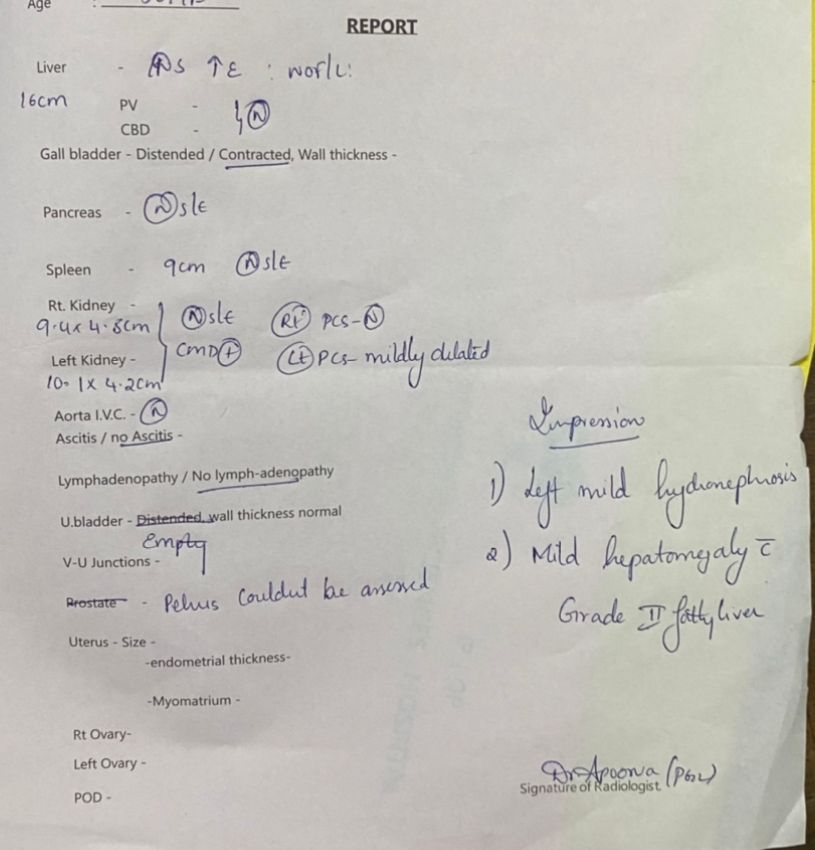
No organomegaly
Percussion:
Dullness over spleen and liver
Auscultation:
Bowel sounds heard.
- CNS examination
No focal neurological deficits
Gait- NORMAL

















Comments
Post a Comment