LONG CASE - FINAL PRACTICALS GENERAL MEDICINE
NAME : M. NAGA VARSHA
BATCH : 2017
HALL TICKET NO. : 1701006102
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
FOLLOWING IS THE VIEW OF MY CASE
A 35 year old male, bartender by occupation, resident of Sathupalli, Khammam district, came to the hospital with the following chief complaints --
- shortness of breath - from 10 days
- cough- from 2 days
- palpitations - from 7 days
- 1 month ago, he developed shortness of breath while lying down, then he visited local RMP, where he was given an injection? and symptoms subside for a while. He experienced symptoms after consumption of alcohol.
- later he visited another doctor, few investigations were done and was told to have a heart problem?
- insidious onset
- mucopurulent
- sudden in onset
- no associated with chest pain
- NO history of similar complaints in the past.
- Not a known case of Diabetes, Hypertension, Tuberculosis, Asthma, hypothyroidism/hyperthyroidism, COPD, and blood transfusions.
- no history of previous surgeries'
- Diet: mixed
- Appetite: reduced from past 10 days
- Bowel habits: normal
- Bladder habits: normal
- Sleep: disturbed from past 10 day
- Addictions:
- Built and nourishment: moderately built and moderately nourished
- Pallor: No pallor
- Icterus: No icterus
- Cyanosis: No cyanosis
- Clubbing: No clubbing
- Generalized lymphadenopathy: No generalized lymphadenopathy
- Pedal edema: No pedal edema
- Temperature afebrile
- Pulse 140-160 bpm (irregularly irregular)
- Respiratory rate : 30 per minute
- Bp 130/90
- Spo2 98%
- GRBS 132 mg%
- The chest wall is bilaterally symmetrical
- No dilated veins, scars or sinuses are seen
- Apical impulse or pulsations cannot be appreciated
- Apex beat is shifted to 6th inter coastal space , 2-3cm deviated from mid clavicular line
- No parasternal heave felt
- No thrill felt
- Right and left borders of the heart are percussed
- S1 and S2 heard
- Shape- elliptical
- B/L symmetrical ,
- Both sides moving equally with respiration .
- Trachea - central
- Expansion of chest is symmetrical.
- Vocal fremitus - normal
- resonant bilaterally
- bilateral air entry present.
- wheeze is present in all areas
- Shape – elliptical
- Flanks – full
- Umbilicus –everted
- All quadrants of abdomen are moving with respiration.
- No dilated veins, hernial orifices, sinuses
- No visible pulsations.
- Apical Impulse is not appreciated
- Chest is moving normally with respiration.
- No dilated veins, scars, sinuses.
Palpation :
- No local rise of temperature and tenderness
- All inspectory findings are confirmed.
- No guarding, rigidity
Percussion:
- There is no fluid thrill , shifting dullness.
- Percussion of liver for liver span
- Percussion of spleen- dull note
Auscultation:
- Bowel sounds are feeble.
4.CENTRAL NERVOUS SYSTEM EXAMINATION:
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N N
Lower limbs N N
TONE
Upper limbs. N. N
Lower limbs. N N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are well appreciated .
- serum creatinine : 1.0 mg\dl
- blood urea : 22mg\dl
- serum electrolytes : Na+ - 138 mEq\L
- K+ - 3.9
- Cl- - 100
- Ph : 7.43
- PCo2 : 26.8 mmHg
- PO2 : 76.3 mmHg
- HCo3: 17.6 mmol\L
- St. HCo3 : 20.4 mmol\L
- TCo2 : 35
- O2 stat : 94.0
- hemoglobin : 12.0 gm\dl
- TLC : 14,000
- PCV : 37.6
- MCV : 70.9
- MCH : 22.4
- RDW-CV : 16.9
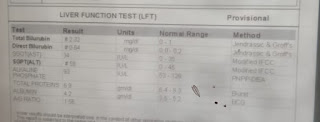
- total bilirubin : 2.32
- direct bilirubin : 0.64
- SGPT : 58
- SGOT : 34
- Ph : 7.43
- PCo2 : 26.8 mmHg
- PO2 : 76.3 mmHg
- HCo3: 17.6 mmol\L
- St. HCo3 : 20.4 mmol\L
- TCo2 : 35
- O2 stat : 94.0
- Hb : 11.3
- TLC : 17,100
- platelets : 3.43
- inj AMIODARONE 900mg in 32 ml normal saline @ 0.5mg\min
- inj AUGMENTIN 1.2gm\IV\BD
- tab AZITHROMYCIN 500mg PO\BD
- inj HYDRODRT 100mg IV\BD
- neb with DUOLIN @ 8th hourly
- inj LASIX 40mg\IV\BD
- inj THIAMINE 200mg in 50ml normal saline IV\TID
- tab CARDARONE 150mg
- tab clopitab 75mg RO OD
- tab ATROVAS 80MG
- Fluid restriction <1.5L per day
- Salt restriction <4gm per day
- Strict temperature chart 4th hourly





















Comments
Post a Comment