35 yr old with Severe Iron deficiency anemia
NAME : M. NAGA VARSHA
BATCH : 2017
ADMISSION NO. 176015
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
FOLLOWING IS THE VIEW OF MY CASE
35 yrs old Male resident of LB nagar, occupation serap dealer came to opd with chief complaints of blood in the stools ,SOB ,easy fatigability ,itching all over the body since 1mn.
HOPI:
Patient was apparently asymptomatic 1mn back then he observed blood in the stools not associated with pain during defecation .
He complaints of easy fatigability,SOB while doing work and lifting little weights also.
History of itching all over the body ,due to itching there are small hyperpigmented patches on both upper and lower limbs since 1mn.
PAST HISTORY:
Similar complaints 1 yr back (blood in stools for 15 days)
N/k/c/o Hypertension, diabetes,asthma, epilepsy,CAD
DAILY ROUTINE:
He wakes up at 5 am and does his daily routine ,eats breakfast at 8:30 and goes to work at 9am , afternoon he takes alcohol and comes home and eats lunch and sleeps until 5 or 6pm ,then again he goes out , drinks alcohol and comes home and does his dinner and goes to bed at 10 pm.
PAST HISTORY:
Similar complaints in the past 1 yr back
Not a k/c/o Diabetes,asthma, coronary artery diseases,epilepsy,thyroid disorders.
FAMILY HISTORY :
Not signigicant
PERSONAL HISTORY:
Diet- mixed
Appetite - normal
Sleep -normal
Bowel and bladder -regular (blood in the stools)
Addictions-
-He is chronic alcoholic since 15 years,
GENERAL EXAMINATION:-
-Patient is conscious, cooperative, with slurred speech
Well oriented to time, place and person
-Moderately built and moderately nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Oedema - absent
VITALS:
B.P:110/70 mmhg
P.R:76bpm
R.R: 22cpm
Temp:99.5 F
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION:
All quadrants moving equally with respiration
No scars, sinuses and engorged veins , visible pulsations.
Anemia due to blood loss by haemorraoids and fissure.
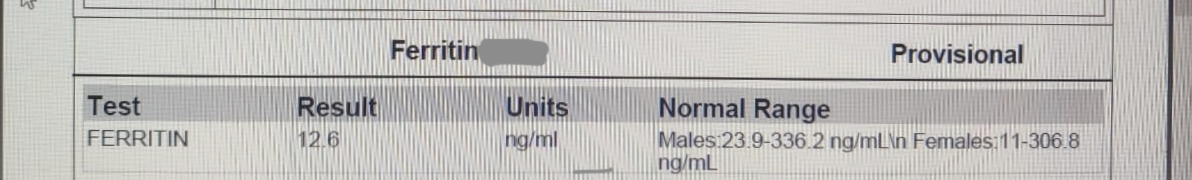
INVESTIGATION:
USG
FINAL DIAGNOSIS:
Anemia secondary to blood loss by haemorraoids (grade 1) and active fissure (11'0 clock)
?IRON DEFICIENCY ANEMIA
Right renal cortical cyst .
TREATMENT
1)T.MONOCEF 200 mg po/BD
2)T.PAN 40mg po/bd
3)SYRUP. LACTULOSE 10ml po/BD
4)OINT.SMUTH
5)SITZ BATH WITH BETADINE -QID
6)HIGH FIBER DIET
7)INJ. VITCOFOL 1.5ml I.M/OD
8)INJ.THIAMINE 100mg in 100 ml NS IV/OD
6/4/2023:



























Comments
Post a Comment